In software, scale once meant sameness. Build once, deploy everywhere. In healthcare, that logic has failed more often than not. A solution that works for outpatient cardiology may break in an inpatient trauma unit. What appears seamless in a rural clinic may require rework in a teaching hospital. AI vendors have learned this the hard way: systems built for uniformity often crash against the complexity of real-world medicine.
The challenge is not a lack of capability; it’s a lack of configurability.
As health systems increasingly deploy ambient and orchestration AI tools, they are discovering a simple truth: clinical work is not monolithic. The roles, workflows, and data contexts in a neonatal ICU differ meaningfully from those in primary care or surgical triage. Yet too many AI solutions have been built as if one interface, one prompt style, or one decision tree can satisfy all clinical users.
According to a recent survey by the American Medical Association, nearly two‑thirds of physicians reported using health‑AI tools in 2024, up from about 38% in 2023. Among these physicians, 57% said that reducing administrative burdens through automation is the biggest area of opportunity. These findings suggest that where tools do not align with existing workflows (how insights are surfaced, how outputs are reviewed, or what user interface elements are used) there is risk not only of underuse but abandonment.
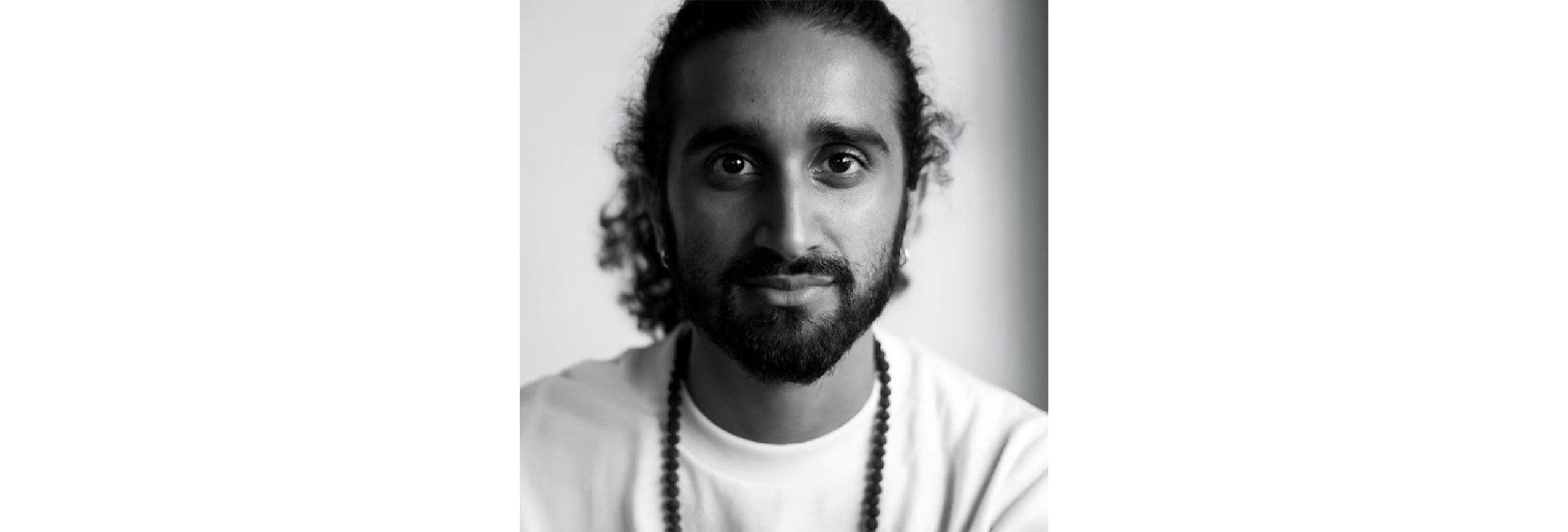
Raj Toleti, founder and CEO of Andor Health, anticipated this years ago. It should come as no surprise that he won EY Entrepreneur Of The Year® 2025 Florida Award in 2025, and also won the same award in 2018. While many digital health startups chased AI novelty, Toleti focused on the harder question: how do you design ambient intelligence and orchestration agents that not only perform, but adapt?
At Andor, that answer has been built into the fabric of ThinkAndor®, a platform Toleti describes not as an “AI app” but as AI infrastructure. It’s agentic, multi-cloud, and brokered: meaning it draws from multiple large language models (LLMs), routes outputs by context, and integrates at the point of care—not in parallel portals or external dashboards.
“In healthcare, AI that can’t flex to the nuances of each role, department, and workflow is destined to fail,” explained Toleti. “The future belongs to configurable intelligence — systems that adapt to clinicians, not the other way around.”
Its most critical feature, however, is configurability by taxonomy.
Rather than assume a single clinical template, ThinkAndor allows customization by department, service line, physical location, role type, and even individual users. In practice, this means that what the platform surfaces to an orthopedic attending in an inpatient setting will differ, subtly but importantly, from what it provides to a nurse in the ED or a telehealth triage assistant. The orchestration agent might emphasize staff coordination in one context; the ambient agent might focus on encounter documentation or observation alerts in another.
This design philosophy stems from Toleti’s broader belief that AI should conform to practice, not force practice to conform to AI.
Nowhere is this more evident than in the way ThinkAndor handles integration. Outputs are not siloed in separate portals or third-party windows; instead, they are embedded directly into the EHR-native environment, ensuring that clinicians interact with AI through the interfaces they already know. Observational, documentation, and orchestration agents are unified, context-sensitive, and, crucially, supervised by humans at every stage.
This role-based design approach improves measurable outcomes, it doesn’t just solve adoption barriers.
For Raj Toleti, this is less a technical abstraction than a core operating belief: AI in healthcare must be fluid, role-aware, and interoperable by design. In 2025, as health systems weigh vendors based on clinical fit, regulatory alignment, and real outcomes — not just innovation theater — this belief is quickly becoming the market standard.
The AI wave is no longer about showing what’s possible. It’s about building what’s sustainable, deployable, and attuned to the fractal realities of medicine. For the systems that succeed, configurability may prove to be the most valuable capability of all.
Written in partnership with Tom White